Bronchiectasis
Fredric Jaffe, Karla M. Criner, Chandra Dass
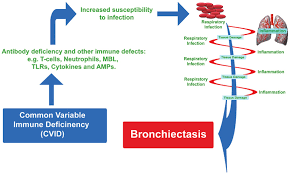
Bronchiectasis is a chronic suppurative lung disease that can be localized or diffuse in nature. It is characterized by dilation of the airways due to a chronic inflammatory process. This process is caused by inadequate removal or clearance of microbes that are present from either an acute or a chronic infection. This disease was first described by Rene Laennec in 1819. He is said to have discovered this disease through auscultation and described the condition through the use of case reports.
Towards a Comprehensive Assessment of Physical Function in Young People with Cystic Fibrosis and Non-cystic Fibrosis Bronchiectasis
Zoe Saynor, Donald Urquhart, Thomas Radtke, Melitta McNarry, Mathieu Gruet
Bronchiectasis is typically associated with considerable morbidity, reduced exercise capacity, and may impact upon quality of life. Children with cystic fibrosis (CF), the most common cause of childhood bronchiectasis, are now living longer than ever before.
In bronchiectasis, poor physical capacity correlates with poor quality of life
Published in European Clinical Respiratory Journal
Patients with bronchiectasis (BE) who suffer frequent exacerbations are likely to experience negative effects on quality of life (QoL) and require more healthcare utilization. We aimed to discover, in a cohort of Finnish BE patients, those risk factors that influence QoL.
Type 2-High Severe Asthma with and without Bronchiectasis: A Prospective Observational Multicentre Study
Published in Journal of Asthma and Allergy
Recently, the coexistence of T2-SA and bronchiectasis (BE) has been considered an emerging phenotype of severe and difficult-to-treat asthma associated with a worse prognosis of the disease representing one of the “treatable traits” highlighted in the latest asthma recommendation. Indeed, the prevalence of BE is significantly higher in SA (range 24–47%) than in mild-to-moderate asthma (3%)
 China
China  Africa
Africa